September 7, 2024
Whats The Treatment For Urinary System Incontinence In Females?
Hormone Adjustments In Females Combined incontinence is an usual kind of urinary system incontinence that numerous females experience throughout menopause, incorporating elements of both stress and anxiety and urge urinary incontinence. This condition can manifest as involuntary leakage throughout physical activities, such as coughing or sneezing (tension urinary incontinence), in addition to an abrupt, strong desire to pee that might lead to leak (urge urinary incontinence). The causes of blended incontinence throughout menopause are usually multifactorial, involving hormone changes that damage pelvic floor muscle mass, age-related bladder modifications, and the cumulative impacts of childbirth. Way of living variables, such as high levels of caffeine and alcohol intake, can substantially impact urinary system incontinence in menopausal women. High levels of caffeine, located in coffee, tea, and some soft drinks, is a diuretic that can boost urine manufacturing and aggravate the bladder, leading to even more frequent peeing and urgency. Alcohol can unwind the bladder muscle mass, harming its capacity to agreement successfully and raising the risk of leakage.- Including anticholinergic medicines can aid in addition to bladder training and fat burning.
- Ins( 1,4,5) P3, inositol 1,4,5-trisphosphate; PKA, protein kinase A; PKC, healthy protein kinase C; PKG, healthy protein kinase G; NO •, nitric oxide; NOS, NO synthase.
- Both most typical kinds of urinary system incontinence that influence women are stress incontinence and prompt incontinence, additionally called overactive bladder.
- For example, your medical professional might prescribe anticholinergics to soothe your bladder if it's overactive.
Urinary Incontinence In Ladies: Challenges And Services
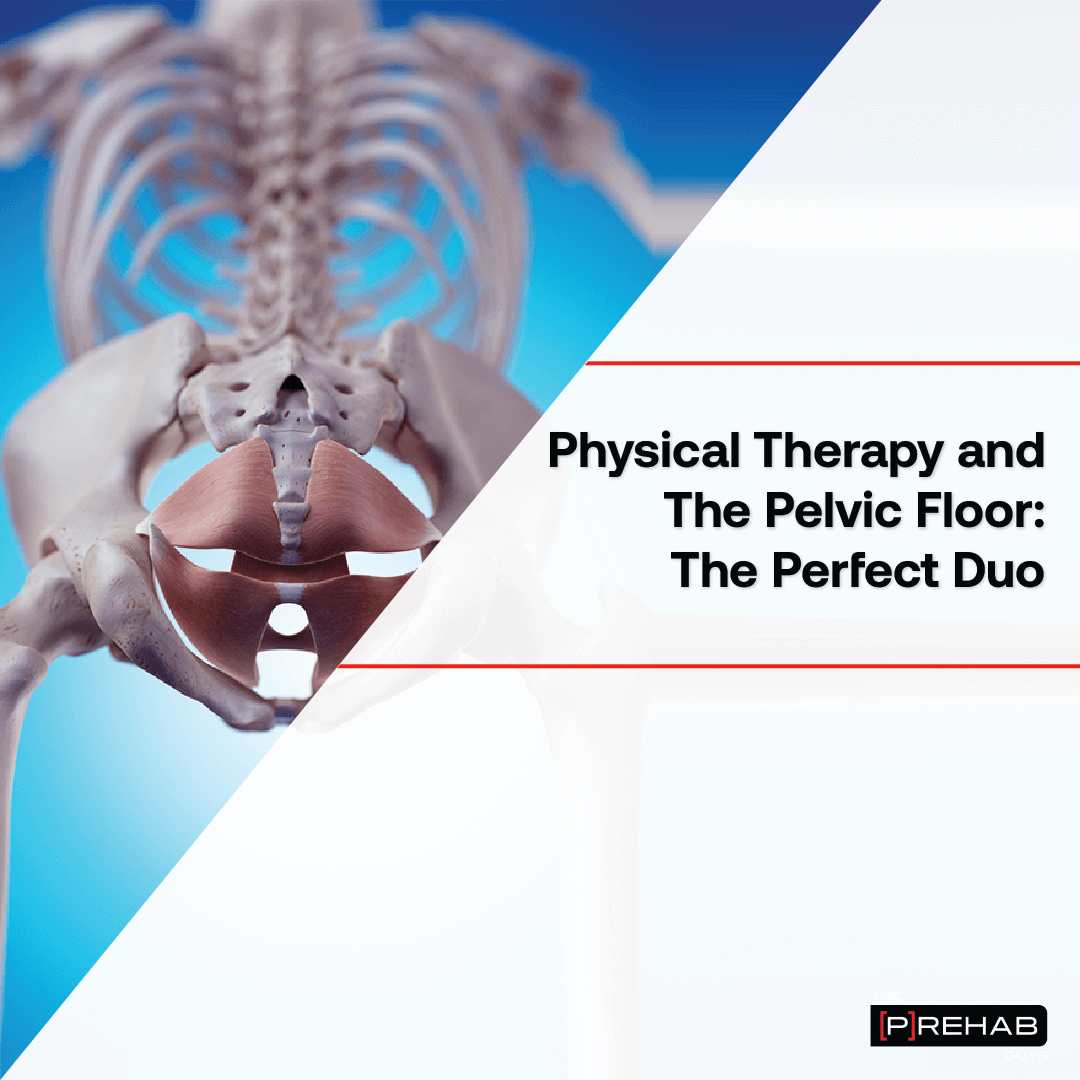
From occasional, small leaks, to more regular rounds of accidents, the sort of urinary incontinence you suffer from can lose a lot more light on its source and just how to treat it. If you are Bladder Control uncomfortable or uncertain about doing Kegel workouts on your own, a medical professional or registered nurse can additionally show you just how to do Kegels. A pelvic flooring physical therapist or other professional might likewise be offered in your location to aid educate you exactly how to reinforce these muscle mass.Qualifying For Cost-free Urinary Incontinence Items
Medical care specialists must consider urinary incontinence a professional top priority and create suitable diagnostic abilities. They must be able to determine and take care of any kind of relevant modifiable variables that might reduce the condition. First-line administration consists of lifestyle and behavior modification, pelvic floor workouts and bladder training. Information given on the Aeroflow Urology blog site is not planned as a substitute for clinical suggestions or treatment from a health care professional. Aeroflow suggests consulting your healthcare provider if you are experiencing clinical issues connecting to urinary incontinence. In addition to women reporting incontinence symptoms during their cycles, new researches are excavating deeper into the impacts the menstruation has on the bladder.Is strolling helpful for incontinence?
Pick tasks that will certainly reduce pressure on your bladder, such as yoga exercise and swimming. Pick reduced impact exercises, such as strolling or Pilates. CHOOSE exercise equipments that do not exert stress on the hips, such as a treadmill or elliptical machine.
Social Links