September 7, 2024
Effect Of Conjugated Estrogen In Stress Urinary System Incontinence In Women With Menopause
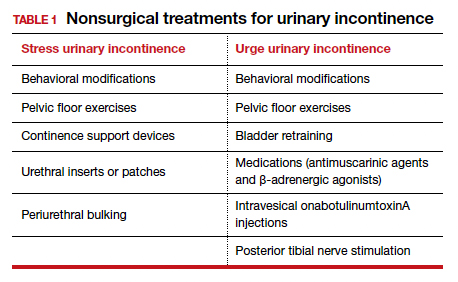
6 Ways To Deal With Bladder Leak They'll first want to try things that have the least influence on your body. Info supplied on the Aeroflow Urology blog is not intended as a replacement for clinical recommendations or treatment from a healthcare specialist. Aeroflow advises consulting your healthcare provider if you are experiencing medical concerns relating to incontinence. Also called Kegel workouts, these exercises can help enhance the toughness of your pelvic flooring. Even if you don't have urinary incontinence, you need to do pelvic floor workouts to assist maintain your pelvic location solid and continent. The change of progesterone and estrogen is why you experience signs and symptoms throughout your cycle and while on your period. This sort of urinary system incontinence causes you to leakage pee when you really feel an urgent demand to pee. Stress urinary incontinence is the most common sort of urinary system incontinence. It can take place throughout workout, coughing, laughing and sneezing. Pelvic floor workouts (Kegels) can reinforce muscular tissues and minimize signs. Some individuals need pessaries, bladder slings or other therapies.Hrt For Prostate Cancer Cells Individuals
These hormone changes can influence bladder function and urinary system behaviors, materializing as urinary system signs such as raised frequency, urgency, or leak. Low levels of estrogen and urinary incontinence go together. As ladies age and start coming close to menopause, the ovaries reduce the procedure of making estrogen, and the levels of this female sex hormonal agent normally decline in the body. [newline] Ultimately, with menopause, the manufacturing of estrogen stops, and this influences the body in several means. Without estrogen, ladies find it hard to preserve healthy urologic functions during and after menopause. Bladder control for ladies starts together with their last menstruation period and raises thereafter.Exactly How Is Urinary Incontinence Dealt With?
Your bladder is like a tank-- as soon as the bladder is full, the brain sends out a signal that it's time to pee. Pee then leaves the bladder when a muscular tissue opens up (sphincter), allowing the urine to flow openly out of the body through the urethra. It is necessary to determine the sort of urinary incontinence that you have, and your signs commonly inform your medical professional which type you have. During this process, the posterior wall surface of the urethra shears off the anterior urethral wall surface to open up the bladder neck when inherent sphincter deficiency is present. Practical incontinence is the inability to hold pee as a result of reasons other than neuro-urologic and lower urinary system system disorder. Videourodynamic research studies are booked to assess intricate situations of stress and anxiety urinary incontinence.- Also stop the circulation of pee in midstream urine causes to enhance the pelvic floor muscles.
- Nocturnal enuresis is one of the most usual pediatric incontinence problem.
- Until recently, estrogen, generally as component of a hormonal agent replacement treatment (HRT) routine, was utilized for treatment of urinary system incontinence in postmenopausal ladies.
- Client advocacy teams provide clients accessibility to info, incontinence products, and doctors that have interest or unique competence in these conditions.
- Urine after that leaves the bladder when a muscle mass opens up (sphincter), allowing the pee to flow freely out of the body through the urethra.
How to clean your bladder normally?
Social Links