September 8, 2024
Menopause And Urinary Incontinence
6 Means To Treat Bladder Leak [23] is labelled the connection in between menopause and urinary system incontinence that women with urinary system incontinence than those that did Fecal Incontinence not have, significantly had higher BMI [24] Health care specialists ought to think about urinary incontinence a scientific concern and create proper diagnostic abilities. They ought to have the ability to recognize and handle any relevant flexible aspects that might ease the condition. Gentle electrical excitement can be efficient for stress incontinence and urge incontinence, yet you may require several therapies over numerous months. Obstructive problems ought to be managed as swiftly as feasible. Urinary system system infection ought to be treated with proper clinical therapy. Ectopic ureters and other congenital anomalies can be operatively dealt with; the medical professional ought to know that useful irregularities of urinary bladder storage or urethral capability may accompany this flaw.Regarding Mayo Facility
In addition, the patient relearns how to control the bladder and strengthen the included muscles. Urinary bladder hypocontractility or poor accommodation of urine throughout storage space may bring about constant leakage of small quantities of pee. Disorder might be triggered by urinary system system infection, chronic inflammatory problems, neoplastic sores, exterior compression, and chronic partial outlet obstruction.How Is Incontinence Dealt With?
These cyclical variations in urinary system behaviors highlight the complex interaction in between hormone fluctuations and bladder feature throughout the menstrual cycle. Speak to your doctor regarding these home therapy options for incontinence before beginning any of them. You may not have the ability to deal with all sorts of incontinence with these lifestyle changes. Your company might additionally make in-depth ideas to you concerning the best way of living modifications to attempt offered your urinary incontinence diagnosis.Overflow Incontinence Pathophysiology
Keeping a healthy and balanced body weight can likewise aid with bladder control. Talk with your doctor about the most effective ways to preserve strong pelvic floor muscle mass throughout your life. Incompetence of the urethral sphincter system (urethral smooth/striated muscular tissue, connective tissue) might arise from nonneurogenic diseases (bladder, urethra, prostate gland) or neurogenic causes.- People with urinary incontinence often live with this problem for 6-9 years prior to seeking medical therapy.
- The hollow member by sustaining muscles is put in a right area and if for any type of factor the sustaining muscle mass shed the capacity, bladder displaced from its location and creates problems for the person.
- As a result, the occurrence of urinary incontinence reported in the literary works is varied.
- Cauda equina disorder can create in patients with a huge centrally sticking out disk.
Just how can bladder leak be quit?
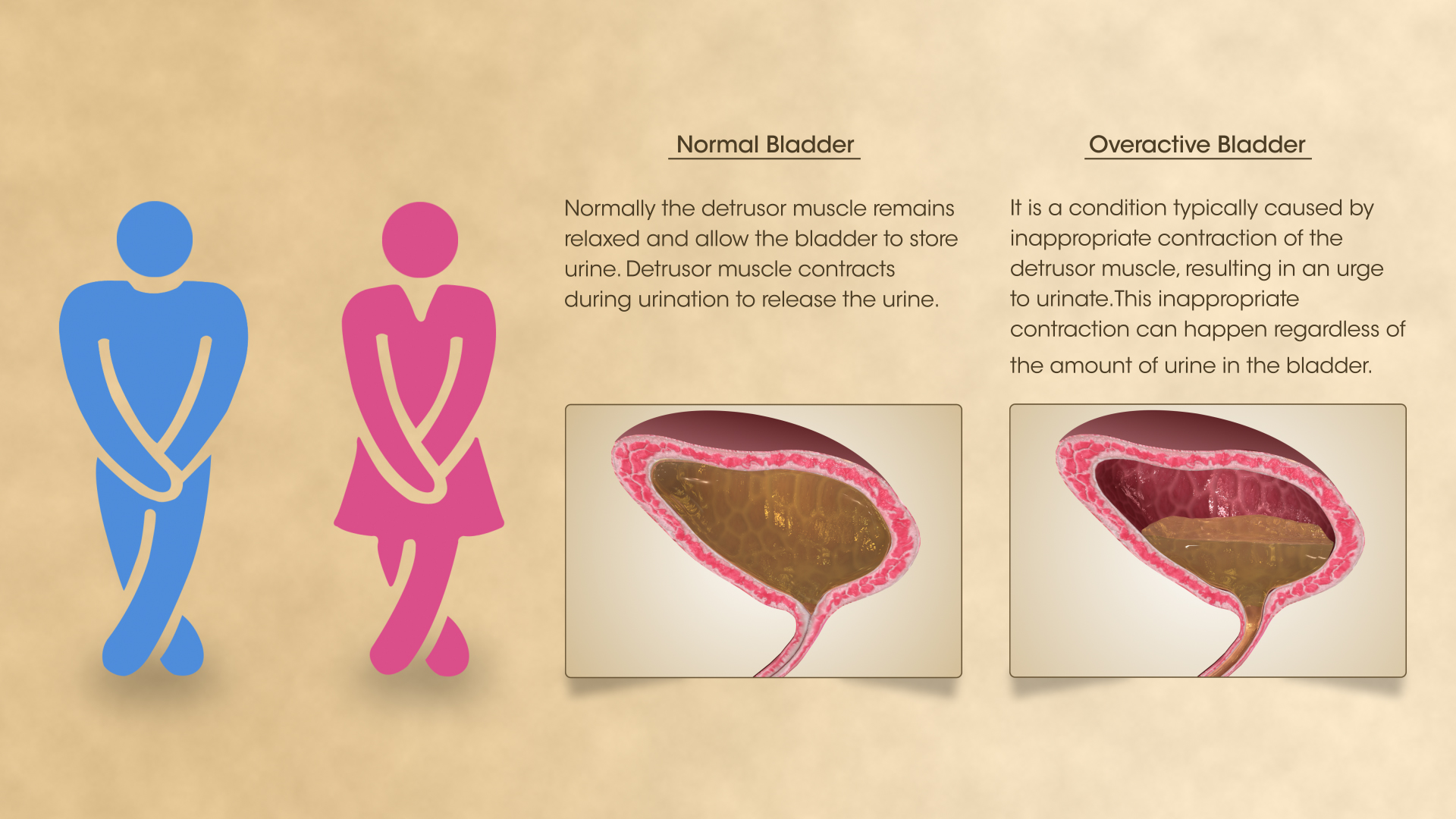
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Applying low-dose, topical estrogen might aid. The medicine comes in the kind of a vaginal lotion, ring or spot. The estrogen might assist bring back the cells in the vagina and urinary tract to soothe some signs. Topical estrogen could not be risk-free for people with a background of bust cancer, uterine cancer or both. Recap. Bladder dysfunction is a common obstacle, particularly later on in life and throughout times of major hormone change. Reduced estrogen bladder signs and symptoms can include incontinence, over active bladder, and discomfort.
Social Links