
August 26, 2024
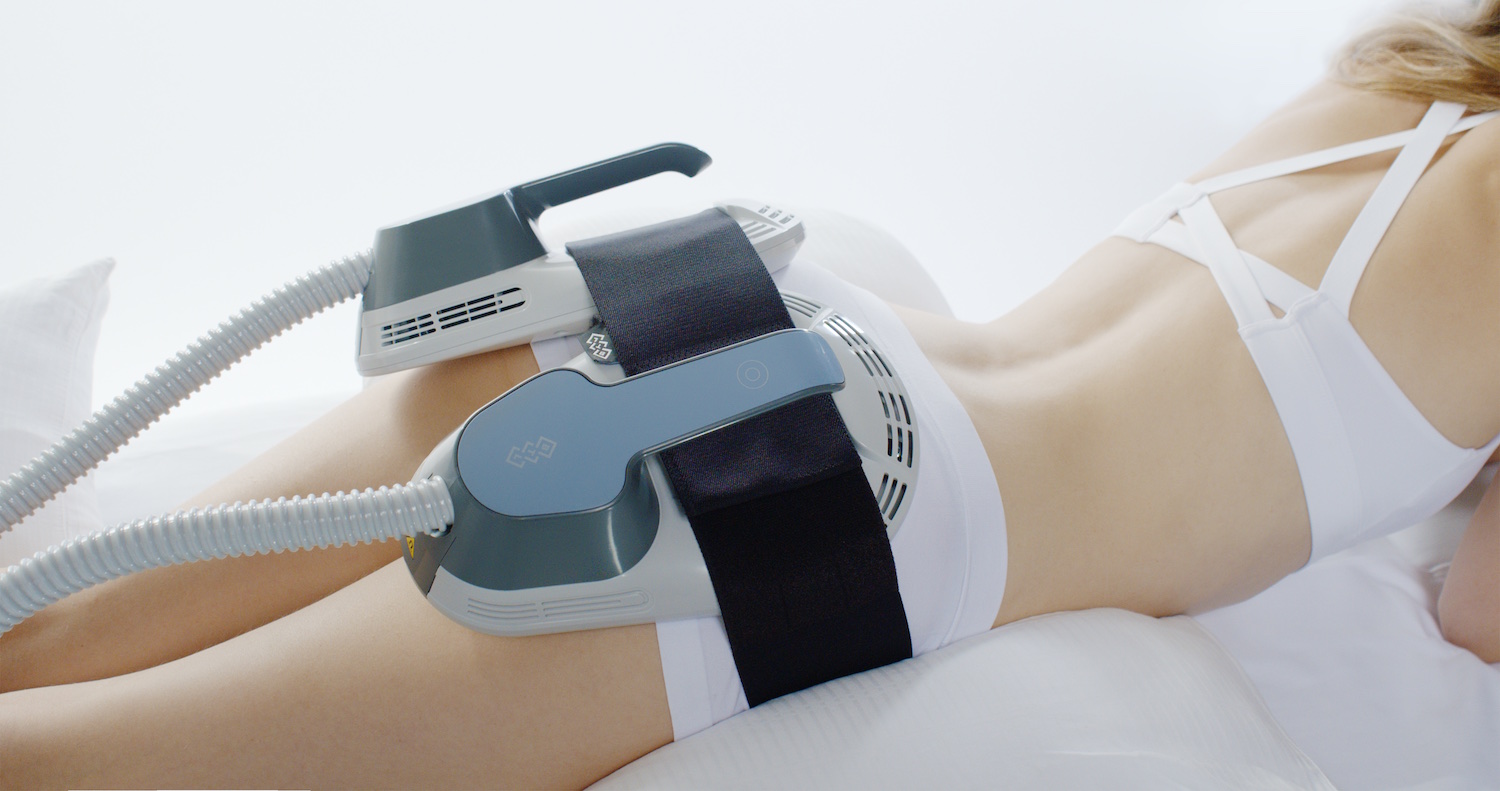
Emsculpt Neo & Cooltone Bend Or Burn Fat And Build Muscular Tissue
Electromuscular Excitement For Urinary Incontinence: Levator 100 Start loading the balloon with isotonic Visit this link contrast, generally to a volume of 0.5 mL. Under online fluoroscopy, press on the bladder with the candid trocar within the U-shaped cannula. If there is movement of the whole bladder, left and appropriate sides together, this is a sign that the urogenital diaphragm has actually not been perforated. If the cystoscope does move, that signifies a place in the appropriate anterior-posterior aircraft.Genital Pessary Usage And Monitoring For Pelvic Body Organ Prolapse
This is done by evaluating the patient totally and includes acquiring a clinical background and a physical examination of the pelvic flooring muscle. Enlightened client permission must be looked for prior to starting treatment. The result of an audit of using the Levator 100 EMS tool, the leader to the newer Levator Turbo CS200, is taken a look at. Radical prostatectomy eliminates the inner urethral sphincter, pubourethral ligaments, and part of the proximal urethral sphincter. The periurethral striated sphincter is mostly responsible for preserving continence after prostatectomy.Similar To Professional Improvement After Essure ® Devices Removal, A Systematic Testimonial
Remove the internal cable and deliver the titanium port meticulously into the developed pocket to the formerly marked level with an Allis clamp, Kelly clamp, or fingers. Next, produce a scrotal pocket using Metzenbaum scissors to produce the subdartos scrotal pocket for the titanium ports. To achieve this, estimate the positioning by putting the ports over the scrotum and noting where the pointer lands on the scrotal skin. This symbolizes the size of tunneling that requires to be carried out. Have an assistant lift the scrotum to the ceiling for counter traction. The scrotal pump can be put through a scrotal cut or tunneled to the scrotum from the abdominal area.Male Pelvic Floor Muscular Tissues
Pelvic radiography or computed tomography must be done to assess balloon placement and volume, as there might be leakage. If this is not the case, a balloon may be leaking, moved out of position, or the initial positioning may not have actually been optimal. A urethral stress profile can be performed with the cuff in energetic and non-active positions. If an underlying condition is creating your symptoms, your medical professional will initially deal with that problem. The major disadvantages consist of postoperative discomfort, longer medical facility keep, and longer bladder catheterization times. Setting a more practical expectation of renovation or "social continence," specified as needing no greater than one urinary incontinence pad daily, significantly improves postoperative satisfaction prices. In circumstances of ongoing urinary incontinence, a 5 mL change in balloon quantity must be made. The advancement of postoperative fibrosis is additionally a contributing factor. After the therapies, cells segmentation revealed a boost inTSCs (103.7%) and CSAs (25.6%) in 11 people, resulting inincreased TSD (69.0%). Urethral tissue degeneration is the most typical source of frequent incontinence due to the loss of cuff compression performance calling for medical revision. This atrophy is generally from chronic cells compression and ischemia, resulting in urethral thinning with a loss of mucosal coaptation and subsequent leak. These procedures occur over an extended period, and individuals report that the sphincter works properly but no longer offers continence. The variety of treatments you need depends on the extent of your urinary incontinence and deteriorated pelvic flooring muscle mass.- When performing this treatment in such individuals, put the trocars slightly much more side to reduce the threat of future disintegration.
- The electromagnetic technology passes through targeted tissues of the pelvic flooring muscular tissues while boosting those muscular tissues and building up toughness.
- Numerous clients observe renovation in their urinary system incontinence after the first treatment session!
- Depending upon the severity of urinary system leak, 0.5 to 1.0 mL per balloon can be included at once.
- Get rid of the lens and bridge of the cystoscope and change them with a blind obturator.
Can EMS help with incontinence?
There are some contraindications to using EMS; nevertheless, when utilized with the best customer for the right conditions, EMS is a risk-free therapy and can improve symptoms of urinary and faecal urinary incontinence, dyspareunia, vaginismus or lax genital muscle mass.

Social Links