September 10, 2024
Menopause And Urinary Incontinence


Pelvic Flooring Exercises
This humiliation should not quit you from dealing with urinary incontinence, however. Typically, your doctor can assist identify the source of your bladder control concern and aid make it better. Speak to your healthcare provider concerning the best means to treat incontinence to make sure that you can lead a full and energetic life without fretting about leakage. The most usual signs and complaints in postmenopausal ladies is exterior genital itchiness. Typically replacement treatment with hormonal agent or estrogen in eliminating itchiness is quite reliable. Distinction of dystrophy from simple degeneration is essential due to the fact that 5 percent of dystrophies of exterior genitalia after years come to be squamous cell cancer [39] Blended urinary incontinence is an usual searching for in older patients with urinary system incontinence disorders. Often, stress and anxiety incontinence signs precede desire urinary incontinence signs in these people.How can bladder leak be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and rest issues.Digestive distress. Applying low-dose, topical estrogen may aid. The medicine comes in the form of a vaginal cream, ring or spot. The estrogen may help bring back the tissues in the vaginal area and urinary system system to soothe some symptoms. Topical estrogen may not be risk-free for people with a history of bust cancer, uterine cancer or both. Summary. Bladder disorder is an usual difficulty, particularly later on in life and during times of significant hormone modification. Low estrogen bladder signs can include urinary incontinence, over active bladder, and pain.
Medical
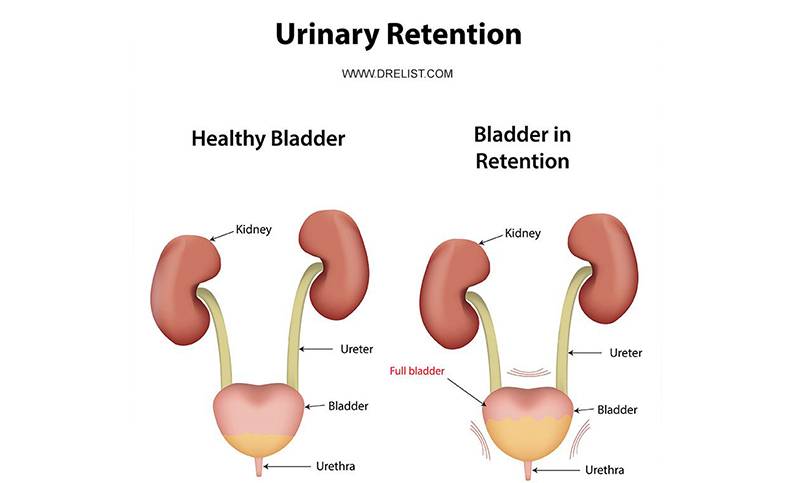
Abdominal, pelvic, and rectal examinations assist identify bigger bladder, anatomic distortions of pelvic body organs, enlargement of prostate, impaction of feces. Comparison studies, as needed, including pneumocystogram (only in the lack of hematuria), contrast urethrogram, and excretory urogram (also called intravenous pyelogram). The frontoparietal electric motor cortex projects to the brainstem knotty formation facilities for micturition, which are responsible for storage and discharge of pee. Sensory nerve cells have stretch receptors in the bladder wall surface that communicate information via ascending spine tracts to the brainstem and somesthetic cortex of the frontoparietal wattles. This pathway is the basis for the assumption of a complete bladder. Various other qualities such as bladder neck setting, urethral length, and concurrent vaginal anomalies may increase the risk of urinary incontinence in women dogs. If clients are incontinent of pee, observe whether sheets and/or the health center dress is stained before a physical therapy session, as these requirement to be altered in order to minimize skin break down. A condom catheter (for guys) or grown-up urinary incontinence undergarments (for males and females) can be applied prior to wheelchair therapy to help in conclusion of the session. From these facilities, reticulospinal systems descend the spinal cord to influence smarts centers in charge of the storage or evacuation of urine. For discharge, the visceral efferent neurons in the sacral sections that innervate the detrusor muscle mass using the pelvic nerves are assisted in. The somatic efferent nerve cells in the sacral segments that innervate the striated urethralis muscle by means of the pudendal nerve are inhibited.- In addition, urinary incontinence is underdiagnosed and underreported.
- A detailed neurologic assessment must be executed in an attempt to establish or rule out a neurogenic reason.
- It might cause more regular urination, pain during sex, vaginal dryness, and other signs and symptoms.
- Animals with peripheral nerve damage enough to cause LMN abnormalities of micturition normally have LMN deficiencies in the perineal location (lowered anal sphincter tone).
Signs Of Hormonal Discrepancy In Women
The aim of this scientific guide is to give an evidence-based method to the monitoring of urinary system incontinence in postmenopausal women. This change in pressure can make your bladder muscular tissues tighten up or loosen up, leading to urinary incontinence signs, such as urinary system retention and leakage. Menopause notes the cessation of ovarian function and a decrease in estrogen and progesterone manufacturing. This hormonal transition, come with by physiological adjustments, can substantially affect urinary system health and wellness and pelvic floor function in menopausal ladies. Progesterone, on the various other hand, influences smooth muscle tone and leisure, possibly affecting bladder function. Key Result Measures Case UI at 1 year among ladies without UI at baseline and severityof UI at 1 year among ladies that had UI at standard. Nocturnal enuresis is one of the most common pediatric urinary incontinence condition. Among one of the most reliable methods to deal with bust cancer cells is early discovery. Ask any type of happy pair what makes their marital relationship a success, and possibilities are they'll tell you this is at the top of the list.Social Links