
September 2, 2024
Stress Incontinence: Causes, Symptoms And Treatment

Pee Incontinence A Review According to the National Organization for Continence, over 25 million adult Americans experience momentary or chronic urinary system incontinence. UI can occur at any type of age, however it is a lot more common amongst women over 50. Urinary system urinary incontinence might be a temporary problem that arises from a hidden clinical condition. It can range from the discomfort of minor losses of pee to serious, frequent wetting. Whether experiencing hormonal changes throughout the age of puberty, menstrual cycle, maternity, or menopause, females can benefit from INNOVO's non-invasive and clinically tried and tested technique to pelvic flooring fortifying.
Therapies That Create Hormonal Agent Signs And Symptoms
Can hormonal agent imbalance impact your bladder?
What Else Can Assist To Decrease Urinary Incontinence?
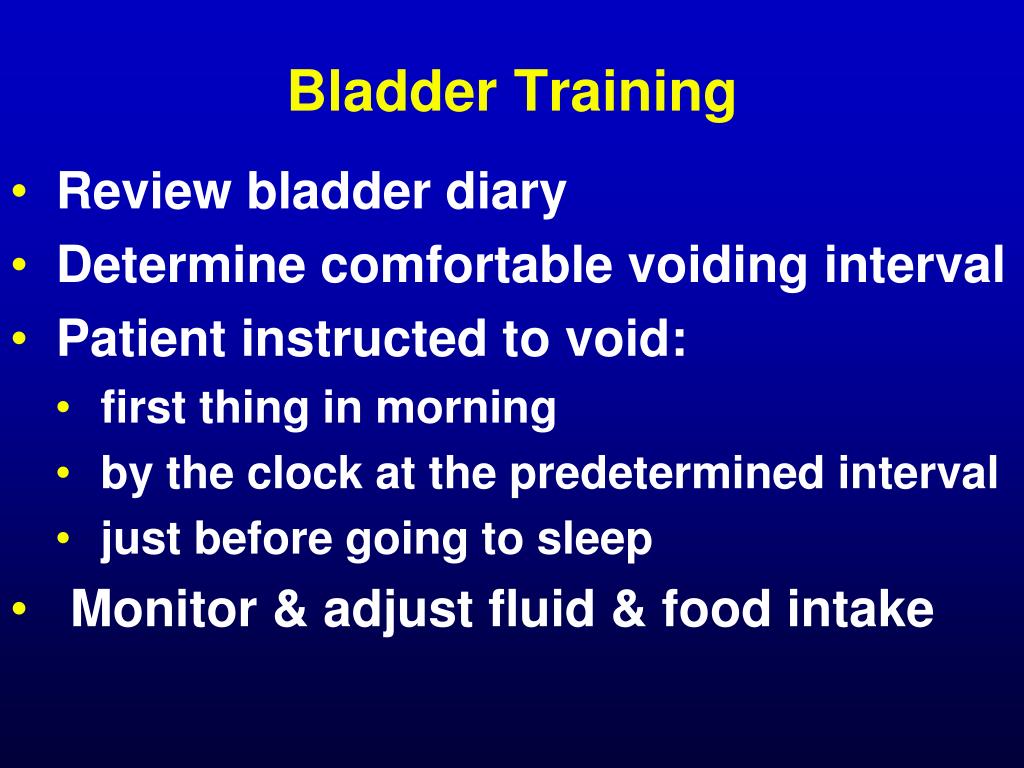
Throughout a female's life, from adolescence to menopause, the delicate balance of hormones manages a symphony of adjustments that can affect urinary system continence and pelvic floor strength. Often, there are adjustments to your daily life that can really aid your urinary incontinence. These changes often include workouts you can do to reinforce your pelvic flooring muscle mass, adjustments to your typical routines and a boosted diet plan. Some individuals see improvements by making these modifications in your home and don't need added treatment. These hormonal shifts can affect bladder feature and urinary habits, showing up as urinary system signs and symptoms such as increased frequency, urgency, or leak. Reduced degrees of estrogen and urinary incontinence go hand in hand. As women age and begin approaching menopause, the ovaries reduce the procedure of making estrogen, and the degrees of this female sex hormonal agent normally decrease in the body. [newline] At some point, with menopause, the manufacturing of estrogen stops, and this impacts the body in lots of methods. Without estrogen, ladies discover it hard to preserve healthy and balanced urologic functions throughout and after menopause. Bladder control for ladies begins together with their final menstrual period and enhances thereafter. Urethral incompetence usually causes periodic urinary incontinence, normally at remainder. Hormone therapy (estrogen) in postmenopausal ladies relieves urinary regularity which leads to enhance in the strength of muscle mass around the bladder. Althoughbasic science in this area is limited, a recent placebo-controlled, randomizedclinical trial of estrogen alone clarifies this problem. Urethral closureis depending on the incorporated Urinary Incontinence Devices Adult Diapers Absorbent Pads Biofeedback Therapy Urology Clinics Continence Specialists Bladder Management Urological Health Continence Products Incontinence Surgery Bladder Retraining Kegel Exercises Urinary Catheters Medication for Incontinence Sacral Nerve Stimulation Incontinence Devices Continence Clinics Overactive Bladder Treatment Voiding Diary Urodynamic Testing Pelvic Floor Muscle Training Pessary Insertion Vaginal Sling Procedures Physical Therapy for Incontinence Electrical Stimulation Behavioral Therapy for Incontinence Urethral Bulking Agents Incontinence Pelvic Exercises Prolapse Management Continence Therapy Bladder Training Programs Botulinum Toxin Injections Lifestyle Modifications for Incontinence Fluid and Diet Management Urge Suppression Techniques Bladder Scanning Continence Care Programs Bladder Neck Support InterStim Therapy Transvaginal Tape Core Strengthening Exercises Pelvic Physiotherapy Pilates for Incontinence Muscle Rehabilitation Yoga for Pelvic Health Postpartum Recovery Programs Strengthening Devices Biofeedback for Pelvic Muscles Pelvic Organ Support Pelvic Muscle Training Aids action of the suburethral genital wall, thepubourethral tendons, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscles that support your pelvic body organs can weaken. This means that your bladder and urethra have much less support-- commonly causing pee leakage. It likewise aids keep your bladder and urethra healthy and balanced and working correctly. They might no longer be able to manage your bladder as they did in the past. As your estrogen levels continue to drop throughout and after menopause, your UI signs and symptoms might worsen. Estrogens, normally in the kind of diethylstilbestrol, are carried out to made sterile females.- The E + P hormonal agents were 0.625 mg/d of conjugated equine estrogen plus2.5 mg/d of medroxyprogesterone acetate (CEE + MPA); estrogen alone consistedof 0.625 mg/d of conjugated equine estrogen (CEE).
- Nerve damages can interrupt signals from your bladder to your brain so you do not experience the urge to pee.
- The pubourethral ligaments additionally suspend the center portion of the urethra to the rear of the pubic bone.
- Estrogen is released in your body before and during ovulation, and thickens the uterine cellular lining to prepare the womb all set for maternity.
- Vasoactive digestive tract peptide, a smooth muscular tissue relaxant, is lowered substantially in the bladders of clients with detrusor overactivity.
- During sacral nerve excitement, an operatively dental implanted tool provides electrical impulses to the nerves that manage bladder activity.
Urinary Incontinence Therapy In Center Tennessee
These cyclical variants in urinary practices emphasize the complex interplay between hormonal changes and bladder feature throughout the menstrual cycle. Talk to your doctor about these home treatment alternatives for incontinence prior to beginning any one of them. You may not be able to treat all sorts of incontinence with these lifestyle modifications. Your service provider might also make detailed ideas to you concerning the most effective way of living adjustments to attempt offered your urinary incontinence medical diagnosis.Social Links